A recent study published in The Lancet Global Health sought to answer this question by comparing trends in contraceptive use and demand for contraception before and during COVID-19 in four geographies in sub-Saharan Africa (SSA).
The first confirmed case of COVID-19 infection in SSA was reported in Nigeria on February 28th, 2020. Although SSA appears to be a notable exception in the global debilitating experience of COVID-19, with total case and mortality burdens lower than the rest of the world, evidence from past emergencies suggests that the pandemic may have long-lasting, detrimental effects on women’s sexual and reproductive health (SRH). Restrictions on movement and service disruptions related to COVID-19 impose challenges on women’s ability to access SRH services, with further consequences, like pandemic-related income loss and school closures, expected to shape women’s health outcomes and behaviors, such as contraceptive use. In the ongoing context of such challenges, women’s access to contraception and risks of unintended pregnancy could be at stake.
In light of this concern, Dr. Shannon N. Wood and colleagues from the Johns Hopkins Bloomberg School of Public Health and partner universities used longitudinal population-level data to examine changes in the need for and use of contraception during COVID-19 in SSA. The study covered four geographies: two at the country-level (Burkina Faso and Kenya) and two at the subnational-level (Kinshasa, Democratic Republic of the Congo, and Lagos, Nigeria). Findings from this study revealed how reproductive health outcomes at the population-level changed during the pandemic, relative to the two years before the pandemic, and shed light on how COVID-19’s SRH impact might vary based on women’s characteristics and life experiences.
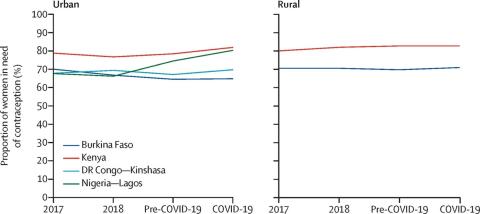
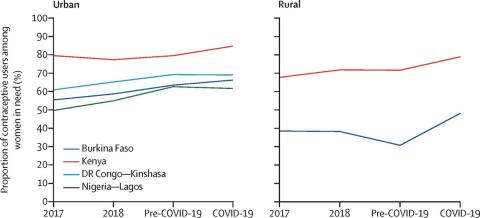
Contrary to the authors’ initial hypothesis, the study found that the proportion of women in need of contraception—that is, women who are married/in-union, sexually active, and want to avoid pregnancy in the next year—increased significantly in Lagos only, by about 6% (rising from 74.5% to 80.3%). When the researchers explored potential changes in contraceptive use, among women in need of contraception, they found that contraceptive use also rose among women in Kenya and rural areas of Burkina Faso since the onset of the pandemic, respectively. No significant changes in contraceptive use were observed in urban sites of Kinshasa or Lagos.
The findings surrounding increased contraceptive use in Kenya and rural Burkina Faso, but not in Kinshasa or Lagos maps to the current method mix in these regions. The authors noted that in the two geographies with an increase in contraceptive use – rural Burkina Faso and Kenya – roughly half of women were using a long-acting method, such as a contraceptive implant, before the pandemic. Fewer women in Kinshasa and Lagos, on the other hand, were using long-acting methods during the study period. This finding underscored an important benefit of long-acting methods in sustaining contraceptive use by choice, even in circumstances characterized by decreased access to services and a spike in commodity shortages. Similar findings about contraceptive dynamics during the COVID-19 pandemic in Kenya and Burkina Faso have been reported in a related study by the same authorship team.
However, the authors also highlighted the ways that these overall population-level findings masked distinct patterns by women’s characteristics. Specifically, the study found that the need for contraception increased among nulliparous women (i.e. women who had not yet initiated childbearing) across all geographies. This finding suggested that women’s desire to have their first child may be delayed during the early stages of the pandemic. Furthermore, in Kenya and rural Burkina Faso, among women with partial income loss due to the pandemic, the researchers observed an increase in contraceptive use. Prior studies have linked economic hardship with women’s changing pregnancy preferences, thus, these changes may reflect a stronger desire to limit or delay childbearing during COVID-19 through the use of contraception.
So, what are the main takeaways?
It appears that on a population-level at least within the initial months of the pandemic, COVID-19 has not brought about the anticipated detrimental effects on women’s access to contraception in SSA. However, the authors “warn against assumptions that women are protected from the future risk of unintended pregnancy, as our reported trends might not be sustainable throughout prolonged economic hardship and service disruption”. As the economic impact of the pandemic unfolds and further lockdown measures are implemented due to spiking cases, greater challenges remain in meeting women’s demand for contraception in the SSA context, requiring concentrated efforts and continued research to ensure women have access to family planning services and are able to achieve their reproductive goals.